The Use of Proton Therapy in the Treatment of Cancers in Adolescents and Young Adults
June 20, 2023
In recent years, the incidence of cancer in adolescents and young adults (AYA)has been climbing. The onset of cancers occurring before age 40 is growing steadily, particularly with cancers of the breast, colon, esophagus, kidney, liver and pancreas. As we move further into the 22nd century and lifespans extend, it is more important than ever to cure young adults, who should otherwise have many decades of life left, with minimal long-term impact of their cancer therapy. Proton therapy is a technology that can help a course of cancer treatment to be just a ripple, instead of the devastating wave treatments have been in years past.
The cause of the increase in cancer incidence in younger people is unclear, but likely multifactorial. Environmental factors, diet, and lifestyle choices all probably contribute. Rates of developing cancer are now higher for each age range than the same age range even 10 years earlier. National Cancer Institute (NCI) estimates state that 4.4% of new cancer cases (about 86,000) will occur in the U.S. in individuals aged 15-39 this year. The NCI also estimates over 9,000 cancer deaths in this age range, accounting for 1.5% of all cancer deaths, with the greatest number stemming from breast cancers (13%), brain and central nervous system tumors (11%), colorectal cancers (10%), and leukemia (10%).
The rates of cancers caused by the human papillomavirus (HPV), also continue to rise. According to the Centers for Disease Control, HPV is the most common sexually transmitted disease in the United States and it accounts for approximately 42.5 million current cases.
Dr. Matthew Ferris
Medical Director, Maryland Proton Treatment Center
Assistant Professor of Radiation Oncology, University of Maryland School of Medicine
Most resolve on their own, but some unlucky people will go on to develop a chronic infection which can eventually lead to cancer. More than 40 strains have been proven to lead to head and neck cancers, anal cancer, vulvar, vaginal, and cervical cancer in women, and penile cancer in men. Fortunately, these cancers are generally very sensitive to treatment and so corresponding cure rates are high, though that means the majority of people will survive and minimizing any long-term treatment related side effects is essential. In 2006, HPV vaccines were first used in the United States, and were originally specified for use in adolescent girls to prevent cervical cancer. As our knowledge of HPV contributing to a wide variety of cancer types grew, the role for HPV vaccination expanded. Beginning in 2011, adolescent males were also recommended for immunization.
Today, people up to age 26 are recommended to receive the vaccine. Adults age 26 to 45 may opt for the vaccination based on their risk of acquiring new HPV infections.
According to the CDC, more than 98% of recipients develop an antibody response to targeted HPV types included in the respective vaccines one month after completing a full vaccination series. The vaccines have been found to have a close to 100% efficacy for the prevention of corresponding HPV-related persistent infections.
Treatments
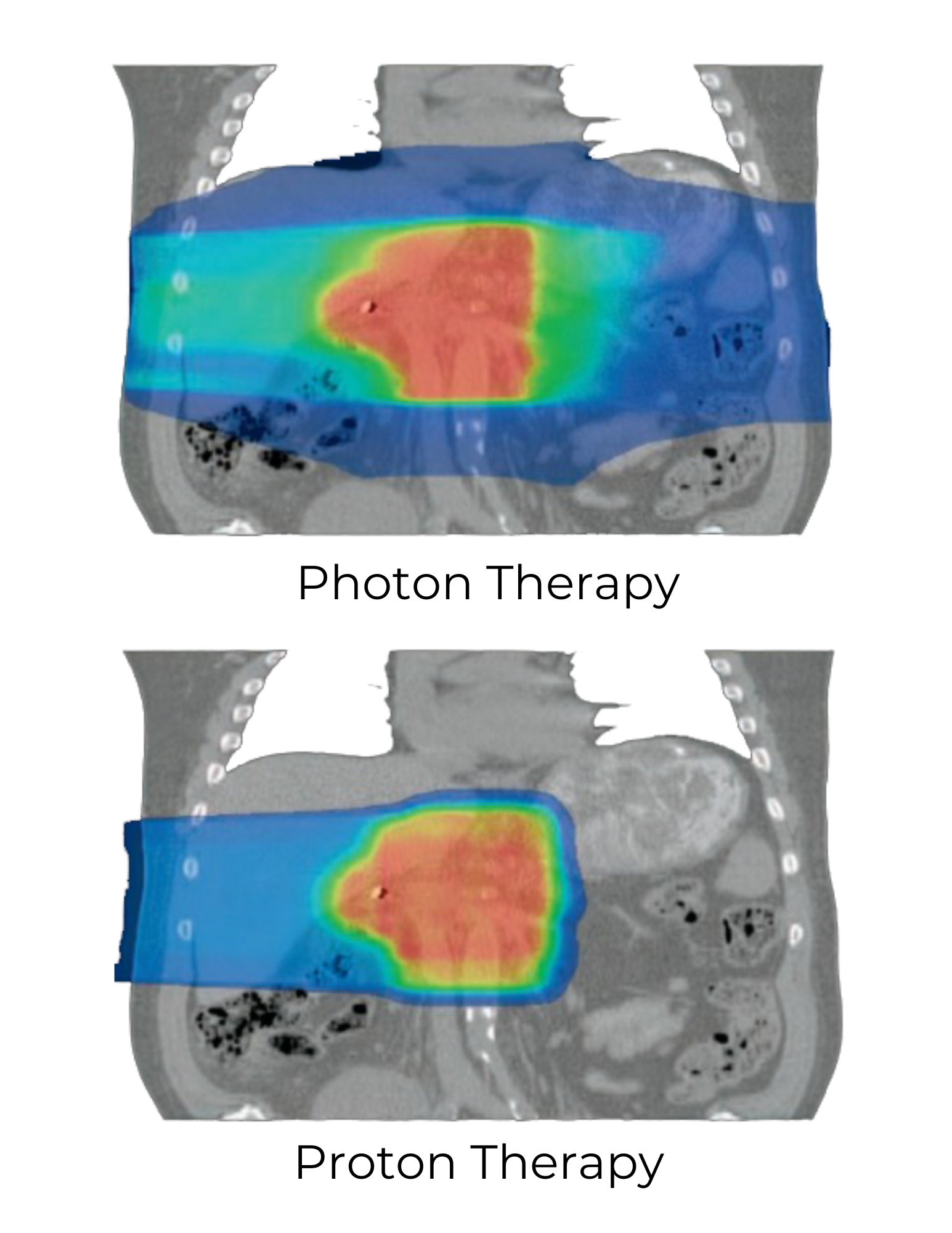
With so much life left to live, it’s critical for AYA to know about the range of treatments available to them. Proton therapy is often the preferred method of delivering radiation therapy to AYA, when radiation therapy is a part of the treatment regimen. Proton therapy takes advantage of particular physical properties of positively charged hydrogen atoms as they interact with tissues in the body—they have the ability to travel to a location and abruptly stop without continuing to pass through. Photons, which are also used to deliver radiation therapy (most centers use photon-based technology), do not have this same ability and continue to pass through the body after they hit their target. So basically, proton therapy allows for therapeutic dose to travel where it needs to with less collateral damage. Nearby normal organs and structures, which do not need to receive the radiation, usually receive less dose with proton therapy, which can potentially be extremely impactful, especially over time. Additionally, the low dose wash—unnecessary dose present with photon therapy just by virtue of the physical properties of photons interacting in the body—is virtually eliminated with proton therapy.
Our knowledge as to exactly how profound the dose advantages seen with proton therapy can be in terms of side effects is still under investigation. Large randomized trials are attempting to describe exactly the amount and degree of side effects which are prevented by using proton therapy, though it will be several years before these trials are concluded, so we look forward to this data being available so we can better counsel our patients the magnitude of what they gain by being treated with protons over photons. For now though, the dose advantages that are obviously apparent are reason enough to routinely offer protons in the AYA population.
Radiation and chemotherapy both can contribute to genetic mutations that may lead to second cancers which develop in the aftermath of cancer treatment (typically years down the line). By using protons and avoiding radiation exposure to unaffected tissues, we minimize the risk of mutations developing in otherwise normal tissue, which over time could develop into another cancer. Our concern for secondary cancer development is highest for the AYA population because their tissues are still growing and dividing. For example, treatment with protons in the brain can help young patients lower the risk of meningioma or glioblastoma development over time. Proton treatment for chest radiation can help young patients avoid secondary breast cancers. In addition to the second cancer risk collateral radiation exposure can cause, collateral radiation to the heart can contribute to cardiac issues or breathing issues, among a number of other problems. Protons have the ability to lower the risk of cardiac disease in the aftermath of chest and breast radiation. In summary, our goal with treatment at MPTC is to preserve quality of life and normal activities as much as possible, both during treatment and in the years to come.
Proton therapy may not always be the preferred method of delivering radiation, but according to the National Comprehensive Cancer Network (NCCN) patients within the AYA population should consider a consultation. Once a patient gets radiation exposure, it cannot be taken back, so doing it right the first time is of extreme importance.



