The Clinical Benefits of Proton Therapy
Clinical Indications
Anal Cancer
Proton therapy reduces dose to the bladder, bone marrow, and bowel, with similar disease outcomes to photon therapy. Longer follow-up time will clarify how this translates to less treatment related toxicity.
- Modiuddin, Adv Radiat Oncol 2021; Ojerholm, Acta Oncol 2015; Nelson, Am J Clin Oncol 2022
Base of Skull
Proton therapy for skull base chordomas is highly effective (local control ~95%) and with limited toxicity severities despite high doses used, and typically close proximity to the brainstem.
- Chhabra, Radiother Oncol 2023
Proton therapy for skull-base chordoma and chondrosarcoma yields low rates of Grade 2 brainstem toxicity (1.3%) despite the high doses utilized (median total dose of 73.8 Gy). Proton therapy can allow for target volume coverage while maintaining point doses to the anterior brainstem to under 64 Gy.
- Holtzman, Acta Oncol 2022
Breast
Proton beam therapy dosimetry yields significant benefit for preventing secondary lung and contralateral breast cancers compared to photon-based techniques.
- Paganetti, Radiother Oncol 2020
Secondary cancer rate odds following breast cancer treatment are significantly lower following proton beam therapy, compared to photon therapy (odds ratio 0.62).
- Xiang, Cancer 2020
With modern proton techniques and planning methods, post-mastectomy pencil beam scanning proton beam therapy demonstrates excellent oncologic outcomes and patient reported outcomes. Side effect rates are favorable compared to photon and older proton techniques.
- Gao, IJROBP 2023
Proton therapy leads to large reductions in dose to almost all relevant normal (uninvolved) organs for bilateral breast cancer cases, and is similarly helpful for patients with previous radiation to the same breast or to the contralateral side.
- Brooks, IJPT 2023
CNS
Proton therapy yields less dose to important brain substructures for adults with brain tumors, which is expected to result in a decrease in neurocognitive impairment in the aftermath of radiation, compared to photon therapy.
- Petruccelli, IJPT 2023
Proton beam therapy results in excellent rates of long-term local control (94%) and low rates of significant side effects (2%) for intracranial meningioma.
- Holtzman, J Neuro Oncol 2023
Proton beam therapy for adult craniopharyngioma is associated with excellent locoregional failure free survival (92% at 5 years) with acceptable toxicity rates despite a typically complicated patient population.
- Beddok, Neuro Oncol 2023
Head and Neck
For oropharyngeal squamous cell carcinomas, the lessened side effects for proton beam therapy yields significantly less work absenteeism and work impairment compared to photons.
- Smith, IJPT 2021
In the aftermath of radiation, quality of life metrics including taste changes and appetite favor proton therapy compared to photon therapy.
- Sio, IJROBP 2016
The lessened side effects with proton beam therapy yields lower rates of feeding tube placement or reliance during or after radiation therapy, compared to photons.
- Blanchard, Radiother Oncol 2016; Manzar, Radiother Oncol 2020
Additionally, there are fewer hospitalizations seen after proton therapy, and less cough and lack of taste.
- Manzar, Radiother Oncol 2020
Proton beam therapy also has demonstrated improved rates of severe mucositis and need for analgesics.
- Yoon, Cancers (Basel) 2021; Manzar, Radiother Oncol 2020
Pencil beam scanning technology dramatically lowers rates of long-term moderate to severe dry mouth compared to photon based techniques (6 versus 20%).
- Aggarwal, Cancer 2021
Proton therapy minimizes excess dose to the mandible and reduces risk of osteoradionecrosis (2% versus 7.7% for photons).
- Zhang, Radiother Oncol 2017
For nasopharyngeal cancer, proton beam therapy results in significantly less acute toxicity burden compared to photon therapy (odds ratio 0.15 of developing grade 2 or higher adverse effect), rare rates of late toxicities, and has excellent locoregional control.
- Li, JAMA Network Open 2021
For nasopharyngeal cancer 60% lower rates of feeding tubes.
- MD Anderson Proton Pals Support Group
For sinonasal cancers it has been projected using photons instead of protons may increase the relative risk of developing a secondary malignancy 3.35x.
- Lewis, Med Dosim 2022
For head and neck reirradiation, proton therapy offers an avenue for disease control and improved outcomes compared to prior series of photon-treated patients.
- Lee, Jama Netw Open 2023
Esophageal
Proton beam therapy reduces the risk and severity of adverse events. Randomized phase IIB study demonstrates significantly lower cardiopulmonary toxicities with protons. Photon patients experienced 2.3x higher total toxicity (side effect) burden and 7.6x higher post-operative complication scores.
- Lin, JCO 2020
Notable improvements in proton dosimetry (heart, lung, spinal cord dose) compared to even advanced photon techniques likely helps to drive these reduced rates of side effects seen with proton therapy patients.
- Cui, Front Oncol 2022
Gynecologic
Whole pelvic proton therapy for gynecologic malignancies (endometrial, cervical, vaginal cancer) yields favorable locoregional control with low rates of significant genitourinary or gastrointestinal side effects.
- Berlin, Gynecol Oncol 2023; Arians, IJROBP 2023
Long term quality of life outcomes approach the normal (untreated) age-matched population for patients with GYN cancers treated with proton beam therapy on the prospective APROVE-trial.
- Meixner, Radiat Oncol 2023
Proton beam therapy reduces dose to the pelvic bone marrow, small bowel, large bowel, and bladder compared to photon therapy, for gynecologic cases in need of para-aortic radiation.
- Xu, IJPT 2018
Proton therapy is considered frequently preferred for advanced or unresectable pelvic tumors with significant pelvic or peri-aortic nodal disease.
- ASTRO Model Policy for PBT, 2023
Liver
Proton beam therapy significantly improves progression free survival and local control (tumor control, 5.64x greater odds of control for protons) for hepatocellular carcinoma compared to transarterial chemoembolization (TACE). Proton therapy led to significantly less need for hospitalization, and a 28% cost savings relative to TACE.
- Bush, Cancer 2023
Per a multi-institutional study of patients with unresectable hepatocellular and intrahepatic cholangiocarcinomas, proton beam therapy local control rates are in excess of 90% at 1 year, due to ability to dose escalate while maintaining low organ at risk dose and thus low rates of toxicity.
- Parzen, Radiat Oncol 2020
Proton beam therapy yields low doses to uninvolved liver, allowing for high, ablative doses to even large or multiple metastatic lesions (such as from colorectal cancer), with subsequent promising rates of lesional control.
- Coffman, J Gastrointest Oncol 2021; Kang, J Gastrointest Oncol 2019
Lung
For locally advanced non-small cell lung cancer, pencil beam scanning proton beam therapy yields significant dosimetric improvements for almost any non-target structure in the chest compared to even the most advanced photon-based techniques. Normal lung, esophagus, heart, and cardiac substructure dosimetry typically demonstrate significant reductions in radiation dose with proton therapy.
- Ferris, PRO 2019
Particle therapy such as proton beam therapy is associated with significantly less severe lymphopenia (low immune system counts) during lung cancer radiation, which is associated with better overall survival. Proton therapy giving less dose to the aorta and thoracic bone marrow (compared to photons) may be the driver behind this.
- Li, IJROBP 2023
Proton therapy is an avenue to re-irradiate radiorecurrent lung cancers with limited toxicity in the modern pencil beam scanning era.
- Janopaul-Naylor, Front Oncol 2023
Lymphoma
Consideration for use of proton therapy encouraged, especially for mediastinal lymphomas,
- NCCN (National Comprehensive Cancer Network), ILROG, and ASTRO guidelines
Despite advancement in photon therapy (VMAT), long term side effects from the unnecessary dose wash given to normal organs for treatment of mediastinal lymphoma cases contribute to excess patient mortality risk, particularly with respect to cardiovascular disease and secondary cancers. Much of this could be mitigated with use of proton therapy.
- Houlihan, Clin Transl Oncol 2022
Proton therapy substantially reduces dose to the heart, lungs, breasts, and circulating blood cells compared to even advanced photon techniques with breath hold. Treating mediastinal (anterior chest) masses with proton therapy using breath hold technique minimizes dose to normal organs more than any other technology available in the US. This is especially critical since many patients with lymphomas in this location are young with highly curable cancers, and have many decades of life left; minimizing dose to normal organs is especially critical. When modeling late effects from radiation such as heart failure, myocardial infarction, valvular heart disease, lung cancer, or breast cancer, one group found treating with protons instead of photons translates to significant improvements in theoretical “life years lost” due to potential side effects from the radiation dose received.
- Patel, Radiotherapy and Oncology 2022; Rechner, Radiotherapy and Oncology 2017
Rates of radiation pneumonitis (lung inflammation) after mediastinal proton therapy are improved for relapsed/refractory lymphomas compared to prior studies of proton patients.
- Tseng, IJROBP 2021
Pancreatic
Proton beam therapy for locally advanced pancreatic cancer typically has dosimetric advantages (less dose to small bowel, liver, duodenum, stomach), is well tolerated, and comparable to photon based techniques in terms of effectiveness. Future studies may elucidate how the dosimetric advantages translate to clinical benefit (less side effects).
- Eckstein, Adv Radiat Oncol 2023; Rapp, J Gastrointest Oncol 2022
Proton beam stereotactic body radiation therapy (SBRT) is typically dosimetrically superior for stomach and duodenal dose for pancreatic head tumors compared to photon based SBRT. This may allow for increased doses to tumor, which may be associated with better tumor control outcomes.
- Liu, Front Oncol 2021; Shin, Cancers (Basel) 2022
Proton beam therapy may be useful for treatment of unresectable tumors.
- ASTRO Model Policy
Pediatrics
Pediatric brain tumor patients receiving proton beam therapy have superior neurocognitive outcomes, compared to patients who received photon therapy.
- Merchant, Lancet Oncology 2023; Lassaletta, World J Pediatr 2023; Mash, Neuropsychology 2023
The majority of proton beam patients who are treated for intracranial tumors demonstrate stability in baseline cognitive function over time.
- Flechl, IJROBP 2023
Proton beam therapy yields excellent tumor control with low toxicity rates and lower projected rates of secondary malignancies in adolescent and young adult patients treated with craniospinal irradiation for solid tumors such as medulloblastoma and ependymoma.
- Vazquez, Pediatr Blood Cancer 2023
Proton beam therapy craniospinal radiation yields less nausea and vomiting compared to photon-based techniques.
- Uemura, Cancer Med 2022
Proton therapy yields significantly less facial deformation as patients grow, following treatment of parameningeal rhabdomyosarcomas.
- Hol, Pediatr Blood Cancer 2023
Whole lung radiation is a component of management of certain pediatric malignancies, and proton therapy has capacity to decrease doses to the heart, coronary substructures, major blood vessels, esophagus, kidney, liver, pancreas, thyroid, stomach, spleen, and breast tissue, compared to photons.
- Cunningham, IJROBP 2023
Treatment of pediatric chordomas with surgery and proton therapy is effective with low rates of late toxicity.
- Loakeim-Ioannidou, Neuro Oncol 2023
Prostate
Proton therapy is associated with significantly reduced odds (odds ratio 0.18) of secondary cancer development for head and neck cancer patients, compared to photon-based radiation techniques.
- Xiang, Cancer 2020
Proton therapy for prostate cancer demonstrates minimal treatment-related toxicities and very good oncologic outcomes.
- Forsthoefel, IJPT 2022; Hasan, Prostate 2023
Prostate patients in need of radiation to the pelvic lymph nodes seem to experience less gastrointestinal side effects during their radiation course compared to photon-based series, which is likely due to less dose to the small bowel.
- Chuong, Acta Oncol 2018
Rectal
Protons offer lower dose to small bowel, bone marrow, and bladder, which can be very helpful for certain rectal cancer cases for which sparing these structures as critical, such as concordant inflammatory bowel disease or prior radiation exposure (re-irradiation).
- Colaco, J Gastrointest Oncol 2014; Koroulakis, Advances in Radiation Oncology 2021
Sarcoma
For soft tissue sarcoma, proton therapy has capacity to maintain appropriate target coverage, similar oncologic and wound healing outcomes, with reduction in doses to adjacent bone, soft tissue, and joints, compared to photon-based techniques which would help limit long term rates of fracture or joint/limb fibrosis.
- Thomas, IJPT 2023; Laughlin, Acta Oncol 2023; Laughlin, IJPT 2022
Favorable dose distribution (lower doses to liver, bowel, and stomach) with low acute side effects is seen for adult patients with pelvic Ewing sarcoma or retroperitoneal sarcomas.
- Schmid, Cancer (Basel) 2022; Chung, Sarcoma 2022
Proton therapy has improved disease control and toxicities for treatment of chest wall, spinal, or paraspinal Ewing sarcoma, compared to historical photon series.
- Indelicato, IJROBP 2022; Indelicato IJROBP May 2022
Proton therapy is effective treatment which minimizes excess dose to nearby tissues and thus keeps toxicities low for treatment of peripheral nerve sheath tumors.
- Bachmann, Front Oncol 2022
Skin
Proton therapy yields less dry mouth, taste changes, and weight loss compared to photon therapy for treatment of skin cancers involving the parotid gland.
- Zarinshenas…Ferris, PTCOG 2023
For locally advanced skin cancers requiring ipsilateral radiation therapy, proton therapy yields lower rates of grade 2 taste changes, oral mucositis, and nausea.
- Romesser, Radiother Oncol 2016
Pencil beam scanning proton therapy is an excellent option for delivering highly conformal treatment in proximity to critical organs at risk for large and advanced skin cancers of the head and neck, particularly with perineural invasion tracking back into the base of skull.
- Holtzman, Oral Oncol 2020
Miscellaneous
In a comparative effectiveness study of 1483 adult patients, proton chemoradiotherapy was associated with significantly reduced adverse events that cause unplanned hospitalizations for patients undergoing concurrent chemoradiotherapy with curative intent for locally advanced cancer. Significantly lower rates of grade 3 or higher toxicities were reduced (odds ratio 0.31), 90-day adverse events of at least grade 2 were reduced (odds ratio 0.78), and declines in performance status were roughly halved (odds ratio 0.51), with use of proton therapy as opposed to photons. This is despite the proton cohort being less favorable in terms of baseline health status.
- Baumann, JAMA Netw Open 2019
NCCN recommends consideration of proton therapy for any AYA (adolescent or young adult) with a predicted risk of radiation-induced late effects to surrounding tissues. Use of proton therapy in this population is also supported by the ASTRO Proton Beam Therapy Model Policy.
- NCCN Guidelines Version 2.2024, Adolescent and Young Adult (AYA) Oncology, https://www.nccn.org/professionals/physician_gls/pdf/aya.pdf
Proton therapy may be especially impactful for patients with radiosensitizing genetic conditions, where minimizing excess/unneeded dose is critical to avoiding late side effects of treatment.
- ASTRO Model Policy
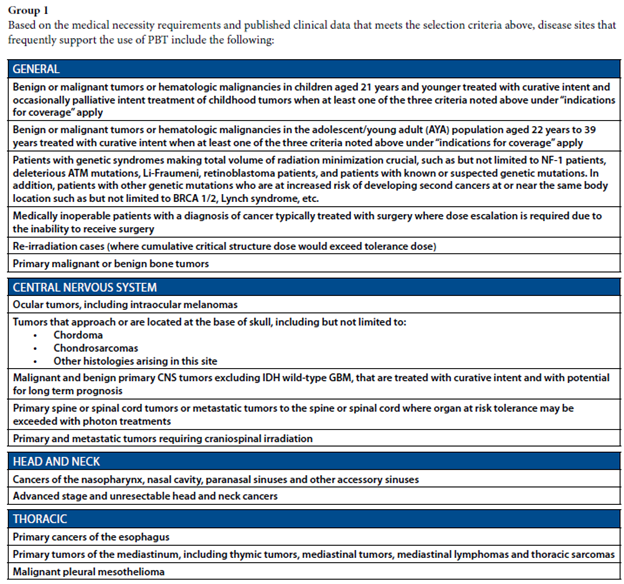
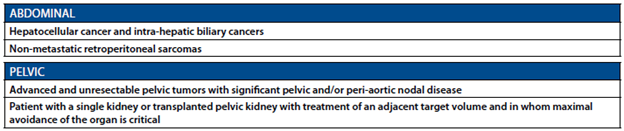
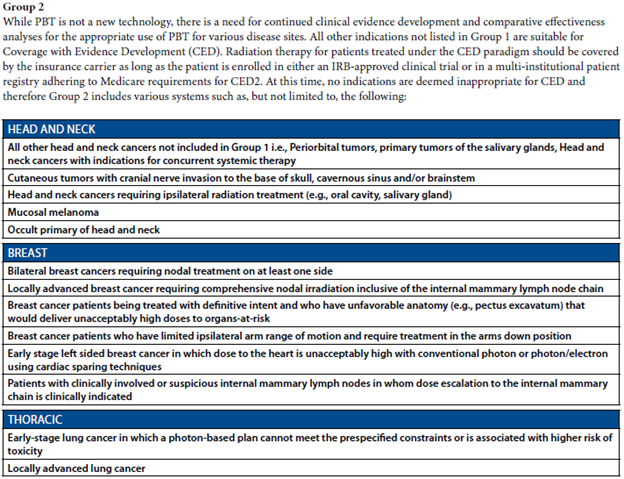
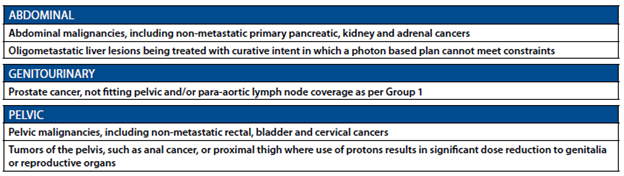
See below for clips from ASTRO Model Policy, 2023.
From ASTRO Model Policy 2023:
Extra to support overall benefits
Breast
Grade 3 skin reactions (Gao, IJROBP 2023) or rib fractures (Bradley, IJPT 2023) are now uncommon with our modern pencil beam scanning technology and are now on par with photon-based techniques, meaning, patients receive the clinical benefits of protons (less heart and lung dose) without the possible drawbacks which were sometimes seen with older passive scatter techniques.
- Gao, IJROBP 2023; Bradley, IJPT 2023
CNS
In a randomized trial, proton craniospinal radiation improved overall survival and CNS progression free survival for patients with non-small cell lung cancer and breast cancer with leptomeningeal metastases, compared to photon therapy.
- Yang, J Clin Oncol 2022
Head and Neck
Proton therapy is associated with significantly reduced odds (odds ratio 0.42) of secondary cancer development for head and neck cancer patients, compared to photon-based radiation techniques.
- Xiang, Cancer 2020
It has been estimated that use of photons over protons may yield up to 4 extra secondary cancer cases per 100 head and neck patients.
- Jain, IJPT 2020
Connect With MPTC
If you’re a physician or medical professional interested in connecting with MPTC, please complete the form below and we’ll be in touch.


