Advances in Prostate Cancer Therapy: The Efficacy of Hypofractionation, Proton Therapy
May 2, 2023
Even though prostate cancer occurs in just half of the population, it’s one of the most commonly diagnosed cancers. According to the American Cancer Society, prostate cancer claims the lives of nearly 35,000 men each year, with more than 288,000 new cases diagnosed each year. In fact, similar to breast cancer, 1 in 8 men will be diagnosed with prostate cancer in his lifetime.
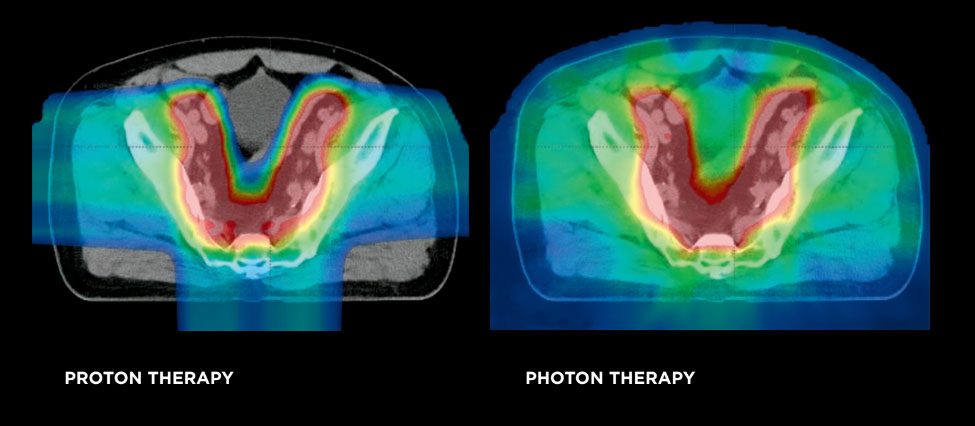
Traditionally, localized prostate cancer was treated with surgery. Now, in the modern area of medicine, another standard treatment is radiation therapy. Radiation therapy is administered through x-rays using beams of photons projected to the tumor and beyond it, while proton therapy delivers a beam of proton particles that are targeted precisely to the tumor. Research data suggests that surgery and radiation are equally effective and most localized prostate cancer is cured with either surgery or radiation. In some cases, when surgery does not elicit a cure, a second treatment is provided, typically in the form of proton or photon radiation.
Radiation therapy is administered daily for many weeks. Empirical and prospective evidence demonstrate that providing a small dose on a daily basis for an eight- to nine-week period is effective to eradicate prostate cancer with minimal side effects. But now, with more advanced targeting and imaging capabilities, like proton therapy and modern-day photon therapy, physicians are turning to an advanced methodology to lessen the time frame.
Dr. Phuoc Tran
Vice Chair of Research, Professor of Radiation Oncology
University of Maryland School of Medicine
Hypofractionation Means More Efficient Cancer Treatments
Studies have evaluated the use of moderate hypofractionation, and the data is clear that it’s similarly effective and well tolerated compared to longer courses of conventionally fractionated treatment. With hypofractionation, the treatment period is reduced by nearly 50% to four to six weeks. Advancing even further, studies are underway to evaluate the use of extreme or ultra hypofractionation in stereotactic body radiation therapy (SBRT), also referred to as stereotactic ablative radiation (SABR). This highest dose can be completed in just five treatments.
Good evidence thus far suggests that results from the implementation of moderate hypofractionation equate to that of conventional radiation therapy. For patients traveling from great distances for therapy who are unable to remain near the clinic for extended periods, ultrahypofractionation provides another option that can be completed in just 10 days.
Hypofractionation is most often utilized for prostate cancers, although other urologic cancers are now being studied. Initial data suggests that hypofractionation could be superior for bladder cancer patients and studies are beginning to evaluate the use of intensive therapies on kidney cancers as well.
With a higher dose, we have the ability, using either protons or highly conformal photons, to better target the dose. So far, the side effects seem to mirror those with traditional radiation levels and the effectiveness seems to be just as positive.
New Treatment of Low Volume Metastasis
In the past, when the cancer was localized, it was considered curable. On the contrary, when the cancer presented as metastatic, it was considered incurable. Radiation was always considered a curative modality and not offered to those with metastatic disease. But today, we’re thinking differently.
Based on results from studies and therapy advancements, we now consider low volume metastasis as a point along the spectrum of disease. There are patients with localized prostate cancer, which is treated with curative therapies, and widely metastasized cancers, that are generally not curable even with modern techniques. We have tended to give these patients more systemic therapy like chemotherapy and hormone therapy as opposed to performing surgery or administering radiation.
Today, we consider metastasis as a spectrum, and those with low volume metastasis – in three to five locations only – as closer to purely localized disease. Active studies are evaluating the efficacy of administering a curative therapy like surgery or radiation for patients with a few lesions, considered low volume, also referred to as oligometastatic. We’re starting to realize that patients who were previously considered incurable may be cured after all.
We can utilize curative radiation, in proton and photon modalities, to have a chance to cure these patients. In these low volume cases, we can provide a highly concentrated radiation dose to the areas in need of exposure, yielding less toxicity for the patient, who previously would have endured chemotherapy throughout the entire body. Radiation was not utilized for more global scenarios due to the risk of exposing normal tissues and organs located adjacent to the affected areas.
Often physicians turn to the Maryland Proton Treatment Center for the most advanced form of radiation therapy, pencil-beam scanning using protons to target prostate cancer tumors with unmatched precision while minimizing damage to healthy tissue. Research studies are on-going to examine whether proton therapy treatment may reduce the incidence of long-term side effects seen with conventional photon treatment, such as an impact on urinary, bowel and erectile function. Fewer side effects during treatment may also allow for increased compliance to treatment.
Proton therapy has been shown to provide minimal side effects on related areas like the bowel and is also less likely to cause a radiation induced secondary cancer, as the surrounding healthy tissues are minimally affected by the precise treatment. Proton therapy is also prescribed for recurrent prostate cancer, in an effort to reduce the risk of side effects and damage to tissues as a result of re-irradiation. In these cases, proton therapy can provide an optimal and tolerable dose of radiation while protecting the healthy tissue surrounding the prostate.