Combatting Recurrent Cancers with Proton Therapy
May 14, 2024
When we care for patients with cancer, the initial treatment involves one or more of the three major modalities – radiation, chemotherapy and surgery. The modalities utilized in the initial treatment are the focus of determining the treatment plan for recurrent cancers.
The good news is that since 1991, cancer mortality rates have decreased by 33%. In addition, we are succeeding at keeping tumors from spreading elsewhere in the body, thanks to tools like immunotherapy and chemotherapy. However, while cancer patients are living longer, the chance for recurrence can be greater. We’re often seeing recurrence of the original cancer at the initial site of treatment.
The reasons for recurrence can vary. Surgery or radiation can create scar tissue in or near the affected area. This can compromise the blood supply as it attempts to reach potential tumor cells remaining at the original tumor site, referred to as the primary tumor site. As a result, chemotherapy and immunotherapy, which travel through the blood stream, may be prevented from fully penetrating tissue spaces and thus failing to eliminate cancer cells at the primary tumor site. This can leave cancer cells behind to spread and net a recurrent cancer diagnosis.
Most often, recurrent cancers occur in the head and neck, brain, esophagus, lung, breast and pelvis, including the rectum, prostate, cervix and endometrium.
Dr. William Regine
Executive Director, Maryland Proton Treatment Center
Professor and Isadore & Fannie Schneider Foxman Chair, Department of Radiation Oncology, University of Maryland School of Medicine
While 60% of cancer patients undergo radiation as part of their initial treatment, whether alone or in combination with surgery or chemotherapy or both, reirradiation presents a challenge. Using traditional photon radiation therapy for a second time at a previously or originally irradiated tumor site limits the allowable dose to the cancerous tissues. This is due to the additional radiation exposure and spillage that would occur to the normal tissues and organs that have already absorbed potentially high and damaging levels of radiation from the treatment related to the initial diagnosis.
Proton Therapy for Recurrent Cancers
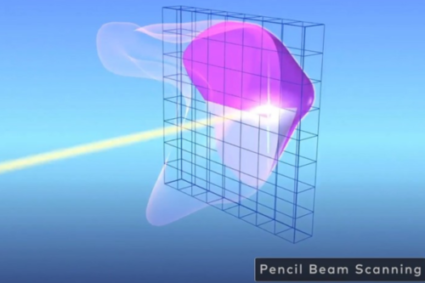
When cancer recurs, the safest and often most favorable treatment option is proton therapy. Proton therapy is a form of radiation that administers positively charged particles directly to the tumor through pencil-sized beams. Reirradiation utilizing protons provides great benefit for the patient. Proton therapy delivers the radiation dose directly to the tumor site, sparing normal, surrounding tissues from additional radiation exposure. This is especially important with reirradiation as surrounding tissues likely endured exposure on the first round of standard radiation therapy using photons.
Using standard radiation for reirradiation limits the dose that we can use due to the repeated exposure of normal tissues to additional radiation by the nature of the way photons work. Therefore, we do not feel comfortable giving as high a dose as indicated to allow for the best chance for a cure. With protons, since there’s not as much spillage, our ability to deliver a stronger dose of radiation that will have a higher likelihood of eradicating a tumor is going to be greater, and, at the same time, we’re exposing less of the normal nearby tissue that’s already been irradiated to additional radiation.
Adding Hyperthermia
Scientific discoveries continue to advance cancer care, providing newer techniques and tools for the treatment of cancers. One such tool is the use of hyperthermia in the treatment of recurrent cancers. Maryland Proton Treatment Center (MPTC), a member of the University of Maryland Greenebaum National Cancer Institute Comprehensive Cancer Center, is the only facility on the East Coast to offer hyperthermia, which uses microwave rays to enhance the effectiveness of proton therapy. Hyperthermia focuses heat equivalent to a low dose fever, about 102° F, at the tumor site to enhance blood flow.
This brings increased blood supply and oxygen to the area, making the delivery of radiation, as well as chemotherapy and immunotherapy more effective. Multiple research studies have shown that the combination of radiation with hyperthermia nearly doubles our ability to control the tumor. Utilizing proton therapy with hyperthermia not only enhances effectiveness but it also spares neighboring healthy tissues.
Hyperthermia can be used with photon and proton radiation. Hyperthermia combined with proton therapy provides the best chance of providing the most therapeutic dose possible for recurrent cancers, while limiting the chance for damaging tissues or organs that have already been irradiated.

This can greatly enhance the chances for a cure.
While hyperthermia has been used for decades, we are using it more and more in combination with proton therapy as we have the ability to conduct non-invasive temperature measurements to ensure accuracy. We no longer need to insert probes deep into tissues to record temperature. Instead, we are using superficial probes that lay on the skin or temporary small catheters in the rectum or bladder. We are able to couple this with MRI technology to generate heat maps to determine the temperature without putting a catheter into the middle of the abdomen or deep into the pelvis.
Hyperthermia can be administered before or after proton treatment.