Turning to Proton Therapy in the Treatment of Thoracic Cancers
March 12, 2024
The use of proton radiation therapy is evolving in the treatment of thoracic cancers, with the most commonly occurring tumors appearing in the lung and esophagus.
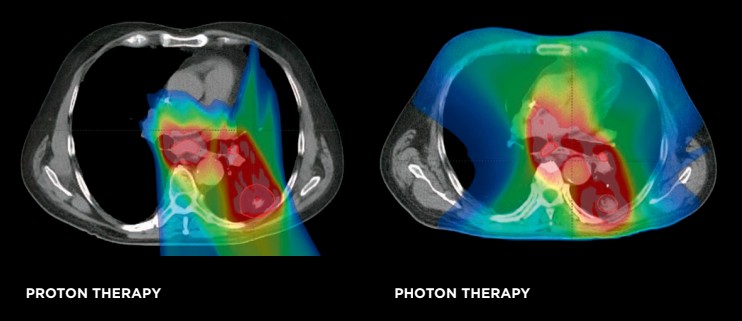
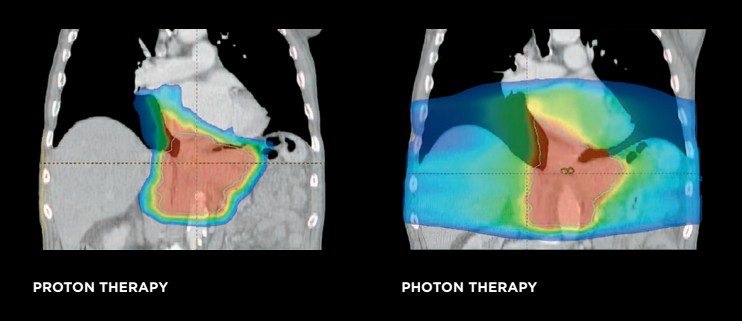
While external beam photon therapy has been the industry standard of care for some time, the evolution of proton therapy, and particularly the modern iteration—pencil beam scanning proton therapy—has yielded an improved ability to treat cancers and spare the normal tissue surrounding them. Protons can approach thoracic cancers, deposit the necessary dose, and abruptly stop, which can limit excess and unnecessary exposure to normal organs in the chest such as the lungs, heart, esophagus, spinal cord and blood cells/bone marrow. The dose reductions with proton therapy can reduce the occurrence of genetic mutations that can accumulate in normal organs following radiation exposure. Additionally, reducing unnecessary radiation dose allows for an improved ability to offer repeat radiation, or re-irradiation, when needed.
Lung Cancer
Ongoing research studies continue to demonstrate that the use of proton therapy has the ability to improve outcomes for non-small cell lung cancer patients.
Dr. Matthew Ferris
Medical Director, Maryland Proton Treatment Center
Assistant Professor of Radiation Oncology, University of Maryland School of Medicine
A study published in February in Radiotherapy & Oncology demonstrates the use of proton therapy to treat lung cancer contributes to lower rates of lymphopenia and anemia compared to photon therapy. Proton therapy yields less dose to the circulating blood in the body, which contains critical white (immune) and red (oxygen containing) blood cells, which are highly radiation sensitive. As a result, the patients who received protons were fitter and more able to receive immunotherapy in the aftermath of chemoradiation. Immunotherapy has improved median survival rates for locally advanced lung cancer patients from around 27 months to almost 50 months, so a patient receiving immunotherapy is critical, and proton therapy seems to help with this.
Proton therapy also delivers less dose to the heart and cardiac substructures, which reduces the chances of a related cardiac event in the aftermath of treatment. Radiation exposure to the heart can lead to arrythmias, myocardial infarctions (acute heart attack from plaque in the coronary arteries), congestive heart failure, pericarditis, and valve issues. Regarding the heart, also, less of a dose to these areas is better, and proton therapy is typically superior than photons in this regard.
Proton therapy has also been shown to provide an avenue, when necessary, for re-irradiation of lung cancers in a safe and effective manner.
The Maryland Proton Treatment Center (MPTC) participated in accruing to a large national cooperative group randomized clinical trial comparing proton therapy and photon therapy for locally advanced lung cancers. The study has recently completed accrual, and the results are anticipated to help further establish clinical benefits of proton therapy.
Esophageal Cancer
A randomized trial comparing proton and photon therapy found that proton therapy reduced the risk and severity of adverse events for patients with esophageal cancers. The total toxicity burden, driven primarily by cardiopulmonary toxicity, was significantly lower (2.3x) for the patients who received proton therapy. Esophageal patients typically undergo chemotherapy and radiation together, followed by surgical resection (esophagectomy) when possible, and the patients on this trial who received proton therapy had lower (7.6x) rates of post-operative complications, and spent less time in the hospital (eight versus 13 days).
Esophageal cancer is an exceptional example of situations for which proton therapy really excels. The large follow-up phase 3 NRG Oncology clinical trial randomizing esophageal cancer patients between protons and photons is expected to continue to emphasize the clinical advantages of proton therapy.
Other (Less Common) Thoracic Cancers
Thymomas and thymic carcinomas are tumors of the thymic gland in the area of the chest just in front of the heart (anterior mediastinum) and radiation therapy is often indicated after surgical resections. Proton therapy is the preferred technique for these cases, as the dose reductions to the heart and cardiac substructures can be quite dramatic. Additionally, in females, dose to the breast tissue is less which can minimize the chances of developing a future breast cancer.
Chest wall sarcomas are another tumor type, that while less common than lung or esophageal cancers, also demonstrate significant advantages in terms of reduction and dose to normal tissues compared to photon therapy.
New Treatment of Thoracic and Other Cancers
The Maryland Proton Treatment Center team is using an advanced technique, proton lattice therapy, for bulky cancers, including large lung cancers and chest wall sarcomas. It is a form of something called “spatially fractionated radiation therapy” and was first implemented at MPTC in the fall of 2023. It delivers high dose spheres into the tumor volume in a 3D grid like fashion, and this provides an excellent way to help with tumor response and allow for improved access of the immune system to bulky tumors.



