Proton Therapy: A Treatment of Choice for Skin Cancer
August 12, 2024
Skin cancer is the most common type of cancer worldwide. About one in five Americans will develop skin cancer by the age of 70, and more than two people die of skin cancer in the U.S. every hour.
The good news is that most patients are successfully “cured” by surgical removal of the cancer when it is detected early.
However, skin cancer comes in different types and has dramatically different degrees of aggressiveness. Surgery alone is sometimes not enough, and sometimes the cancer is located in such a delicate location that surgery would be associated with significant cosmetic impact. For example, a patient with a large or aggressive cancer on the face would be a candidate for post-operative radiation to reduce the risk of local recurrence.
Fortunately, there are advances being made all the time, and now we have additional tools in our arsenal to further our understanding of which skin cancers are the most aggressive and more nuanced. Castle Biosciences’ DecisionDx-SCC, for instance, runs a test on the biological profile of 40 genes within cutaneous squamous cell carcinomas that can help us make decisions such as the need for post-operative radiation or other scans to rule out spread elsewhere throughout the body.
Dr. Matthew Ferris
Medical Director, Maryland Proton Treatment Center
Assistant Professor of Radiation Oncology, University of Maryland School of Medicine
Additionally, we now have a new radiation technology available—pencil beam scanning proton therapy—that has become extremely useful for many skin cancer cases. Thus, when we do have to deliver post-operative radiation, a more sophisticated way of delivering it is available.
Radiation has been used for years either post-operatively or as a replacement for surgery if the cosmetic or functional impacts of surgery will be too significant. Electron therapy and photon therapy have been effectively utilized for decades and are widely available. Still, these techniques are limited by the physical properties of the particles they use to deliver the radiation.
Electrons are useful in treating shallow, superficial areas, but are challenging in handling curved or complex surfaces, or penetrating deeply when needed. Photons can penetrate deeper than electrons and there is occasionally more ability to shape the beam. Additionally, once photons penetrate tissues, they stop very slowly, exposing the underlying tissues to unnecessary radiation dose.
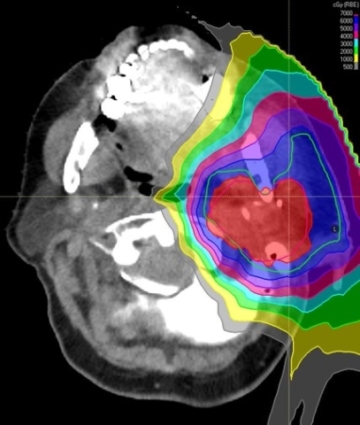
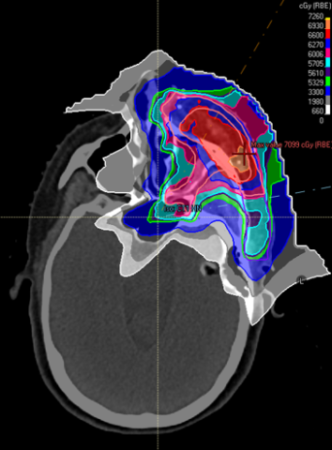
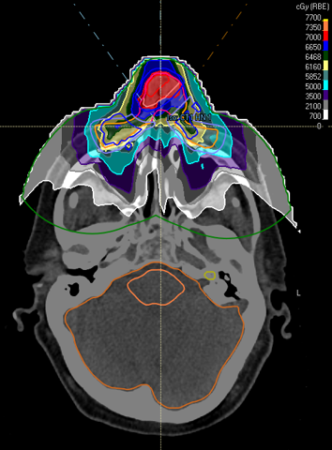
Proton therapy, however, incorporates the individual advantages of other technologies without the drawbacks. The radiation oncologist has exceptional control over where the dose is distributed. The properties of the proton particle allow the dose to be shaped as needed along complex surfaces, to the depth desired, and then abruptly stop.
This is largely due to a fascinating property of protons interacting in the body called the Bragg peak. Depending on the energy you give a proton, it will travel to a certain depth in tissue and stop on a dime.
What does this mean for the individual patient? It means exceptional dosing of the area that needs to be covered, with less likelihood of side effects. When treating on the head or face, this could mean less dose to the eye, lacrimal gland, salivary glands, and mouth.
Therefore, whether the patient needs treatment after a surgery like Mohs, or whether the patient is best suited for radiation therapy alone without surgery, proton therapy is a sophisticated option that often makes both the patient’s and the radiation oncologist’s lives easier with its ability to paint dose to a precise, targeted and complex distribution perfectly tailored for the needs of that particular patient.
We treat squamous cell carcinomas, basal cell carcinomas, melanomas, and Merkel cell carcinomas with proton therapy. We also are part of multi-disciplinary cancer teams (head and neck, skin) from which we can draw additional expertise when needed, such as consideration for other treatment modalities such as immunotherapy.